
Gut Feelings: Why Your Digestion Holds the Key to Health
(Helsinki, 2025-06-19, By Anita Wasik, PhD, DipHM (Medical Herbalist & Biomedical Scientist, Author: Healing the Gut: A Comprehensive Guide)
We often think of digestion as a quiet process happening behind the scenes—food goes in, nutrients are absorbed, and life carries on. But what if your gut is more than just a food processor? What if it’s a powerful control center, influencing everything from your immunity and metabolism to hormone balance, mental clarity, and emotional resilience [1]?

A balanced, well-functioning gut is the cornerstone of vibrant health. But when gut function is compromised—due to poor diet, chronic stress, environmental toxins, infections, or medications—the effects are widespread. Chronic inflammation, nutrient deficiencies, autoimmune disorders, allergies, and metabolic issues often follow [1].
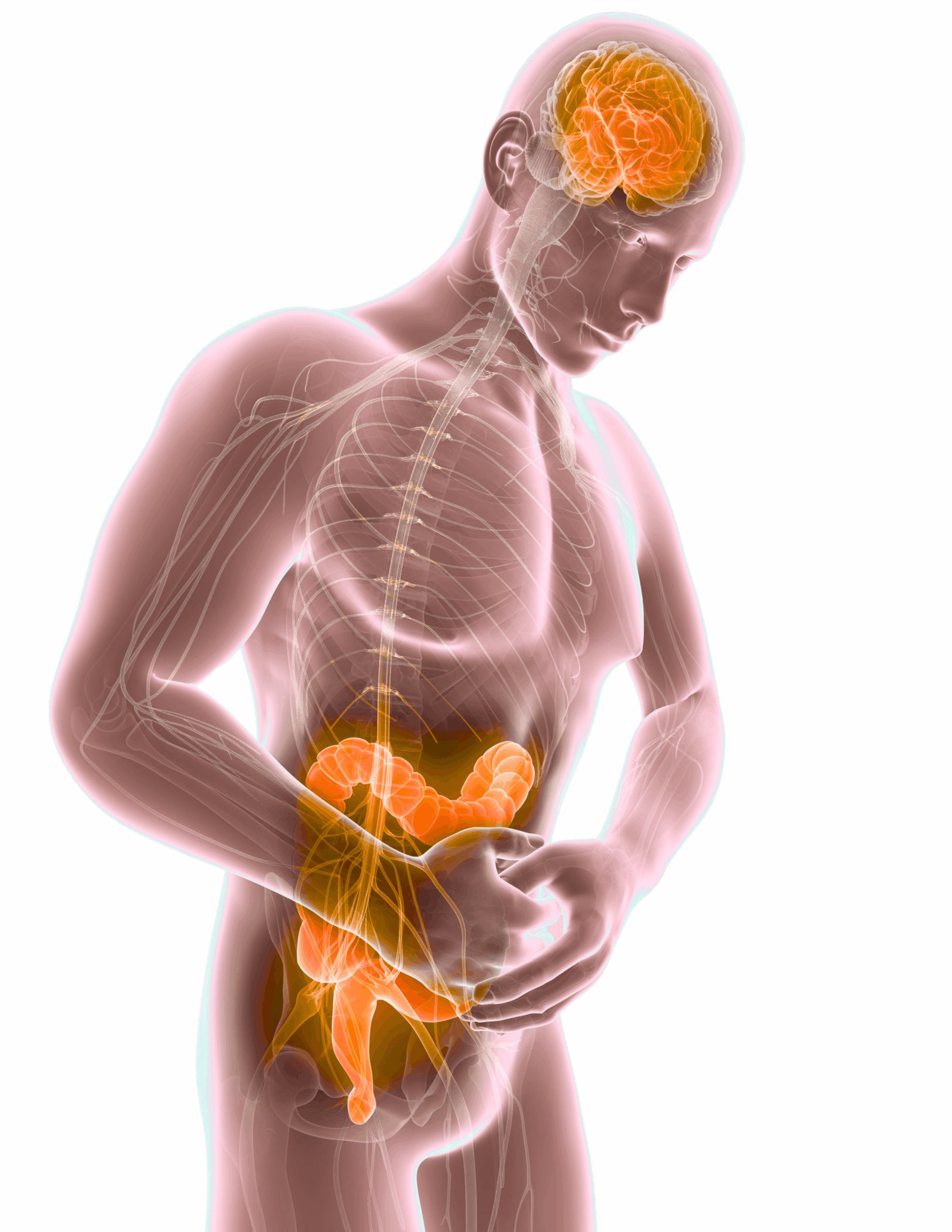
The Forgotten Brain: How Your Gut Talks to Your Mind
You’ve likely heard the phrase “gut feeling.” There’s a reason for that. Your gut is lined with over 100-500 million neurons—so many that scientists call it the second brain. This enteric nervous system communicates with your brain via the vagus nerve and influences your emotional state through neurotransmitters like serotonin and GABA. In fact, around 90% of your serotonin—the “feel-good” neurotransmitter—is produced in the gut [2-5].
This communication is bidirectional, meaning that it functions in two directions. The brain affects our gut function via the sympathetic (‘fight or flight’) and the parasympathetic (‘rest and digest’) nervous systems. The balance of signals from these two inputs affects digestion, secretion of digestive enzymes, absorption of nutrients, the speed at which food moves through the digestive system, and level of inflammation in the gut. On the other side, the gut and its microbiota communicate subtle changes within the gastrointestinal tract to the brain impacting its function and our behaviour. Disturbance in the gut-brain axis is believed to be involved in the development of several gastrointestinal disorders, as well as brain and mental diseases including anxiety, depression, autism, or Parkinson’s [2-5].
A significant part of this communication process is due to the presence of gut microbiota—a complex and diverse community of microorganisms, including bacteria, viruses, fungi, and other microbes—that reside in the gastrointestinal tract [6–8]. In fact, your gut contains about 10 times more microorganisms than human cells and harbors approximately 150 times more genes than the entire human genome. Collectively, the microbiota in your gut weighs an impressive 1–2 kg [9–10]. These tiny organisms play a critical role in your health and well-being by [11–12]:
- Breaking down complex carbohydrates, fiber, and other food components, aiding in nutrient and energy extraction
- Fermenting certain carbohydrates and producing short-chain fatty acids (SCFAs) that support gut and overall health
- Training and regulating the immune system
- Regulating inflammatory processes
- Producing essential vitamins and metabolites
- Supporting metabolism and brain function.
Modern Life, Ancient System: Why Today’s Lifestyles Disrupt the Gut
Millions of people today struggle with unexplained, chronic health issues. While symptoms may vary—from fatigue and brain fog to skin problems, joint pain, or hormone imbalances—many of them have one thing in common: a dysfunctional gut [1].

The catch? Gut issues don’t always present with obvious digestive symptoms. You might feel fine after eating, yet still experience symptoms rooted in inflammation, leaky gut, or dysbiosis (imbalanced microbiota).
Several factors contribute to gut dysfunction, but our modern lifestyle is one of the biggest culprits. The choices we make every day—what we eat, how we manage stress, and even how we sleep—can either support or weaken the integrity of our gut lining [1].
Our ancestors didn’t eat processed food or microwave meals. They didn’t sterilize their environments with chemicals. They lived in sync with the natural world—and their guts thrived. Today, highly processed foods, artificial additives, and lack of fiber all chip away at gut integrity. We sterilize our homes, overuse antibiotics, and live disconnected from nature—conditions that set the stage for harmful microbes to thrive.
But it’s not just about food. Environmental toxins such as pesticides, heavy metals, and mold further disrupt the gut barrier and microbiome. Add in sleep deprivation, inactivity, and unresolved stress, and you have a perfect storm for chronic digestive and systemic illness [1].
Where Natural Medicine Meets Modern Science
As a medical herbalist and scientist, I view gut healing as both an art and a science. Herbal medicine offers time-tested tools—like slippery elm to soothe the lining, bitter herbs to stimulate digestion, and antimicrobial plants like oregano to reduce overgrowth of harmful bacteria.
Science now backs what traditional medicine has long known. We have clinical research on probiotics, polyphenols, intestinal permeability, and gut-brain signaling. But information alone isn’t transformation. The real healing happens when we apply both ancient wisdom and modern evidence in a personalized, holistic way.
The New Era of Gut Healing: A Whole-Person Approach
Healing the gut is not a one-size-fits-all process—it requires a comprehensive, layered approach that looks at the whole person. It begins with eliminating what doesn’t belong: irritants such as inflammatory foods, gut pathogens, and chemical and mold exposures that disrupt the internal environment. Creating this clean slate is essential to calm inflammation and allow the gut lining to begin repairing itself.
Once the immediate stressors are removed, the next focus is on rebuilding the digestive system’s natural capacity. That includes restoring optimal levels of stomach acid, bile, and digestive enzymes so that nutrients can be properly broken down and absorbed—fueling the body’s ability to heal from within.
Rebalancing the microbiome is also critical. This means introducing beneficial bacteria through probiotics and prebiotic-rich foods, as well as fermented options that help repopulate the gut with microbes that promote resilience and harmony. Alongside this, certain nutrients like L-glutamine, zinc, collagen, and specific herbal remedies work deeply to strengthen and seal the intestinal lining, reducing permeability and reversing the symptoms of what’s commonly referred to as leaky gut.
But gut healing isn’t just about what we eat or take—it also depends on how we live. Long-term success requires addressing the lifestyle patterns that either support or sabotage gut health. Managing stress, prioritizing quality sleep, moving your body, and reducing toxin exposure all play a vital role in helping the gut maintain its integrity over time.
When all these pieces come together—physical, emotional, and environmental—a new level of health becomes possible. Through this holistic lens, gut healing transforms from a temporary fix into a sustainable way of life [1].
Beyond the Physical: The Emotional and Energetic Layers of Gut Healing
Conventional medicine often treats health in isolated systems, focusing on symptom relief. But true, lasting healing recognizes the deep connection between mind, body, and spirit.
While dietary and supplement protocols are essential, they may not be enough on their own. The gut is intimately connected to our emotions, energy flow, and spiritual health. Physical symptoms like bloating, sensitivities, or chronic inflammation can stem from unresolved emotional trauma, limiting beliefs, and energetic blockages.
Holistic healing acknowledges the body as an interconnected system. By integrating practices like breathwork, meditation, energy therapy, and emotional processing into physical healing protocols, we treat the whole person—not just the symptoms. This deeper approach often reveals the real root causes of dysfunction and opens the door to transformative health.
About the Author:
Anita Wasik PhD, dipHM is a medical herbalist, biomedical scientist, and educator specializing in chronic and environmental illnesses. Her latest book, Healing the Gut: A Comprehensive Guide, explores gut healing through herbal wisdom and modern science.
References
- Wasik A. Healing the Gut. A Comprehensive Guide. 1st ed. Anita Wasik PhD; 2025.
- https://www.anitawasik.com/post/gut-brain-communication
- Carabotti, M., Scirocco, A., Maselli, M.A. and Severi, C. (2015). The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol. 28(2): 203-209.
- Mayer, E.A. (2011). Gut feelings: the emerging biology of gut-brain communication. Nat Rev Neurosci. 12(8):453-466.
- Cryan, J.F. and Dinan, T.G. (2012). Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci. 13(10):701-712.
- Patel RM, Myers LS, Kurundkar AR, Maheshwari A, Nusrat A, Lin PW. Probiotic bacteria induce maturation of intestinal claudin 3 expression and barrier function. Am J Pathol. 2012 Feb;180(2):626-35.
- Sánchez de Medina F, Ortega-González M, González-Pérez R, Capitán-Cañadas F, Martínez-Augustin O. Host-microbe interactions: the difficult yet peaceful coexistence of the microbiota and the intestinal mucosa. Br J Nutr. 2013 Jan;109 Suppl 2:S12-20.
- Natividad JM, Verdu EF. Modulation of intestinal barrier by intestinal microbiota: pathological and therapeutic implications. Pharmacol Res. 2013 Mar;69(1):42-51.
- Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI. Host-bacterial mutualism in the human intestine. Science. 2005 Mar 25;307(5717):1915-20.
- Gill SR, Pop M, Deboy RT, Eckburg PB, Turnbaugh PJ, Samuel BS, Gordon JI, Relman DA, Fraser-Liggett CM, Nelson KE. Metagenomic analysis of the human distal gut microbiome. Science. 2006 Jun 2;312(5778):1355-9.
- Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Nageshwar Reddy D. Role of the normal gut microbiota. World J Gastroenterol. 2015 Aug 7;21(29):8787-803.
- Rowland I, Gibson G, Heinken A. et al. Gut microbiota functions: metabolism of nutrients and other food components. Eur J Nutr. 2018 Apr 57:1–24.